Your Complete A-to-Z Guide to Diverticulitis
CUSTOM JAVASCRIPT / HTML
If you’ve been diagnosed with diverticulitis, you probably have plenty of questions, like “What is it?” “How did I get it?” and “Do I need to change my diet?”
We’ve got the answers to these questions, and many others you might have about this fairly common disease.
Read our complete guide to learn everything you need to know about how diverticulitis is diagnosed, prevented, treated, and managed.
1. Overview

What Is Diverticulitis?
Occasionally, people develop small, pea-sized pockets(1) in the lining of their bowels. Usually, these pockets are caused by pressure from gas, waste, or liquid on weak parts of the intestines. These “pockets” are called diverticula (plural), and the condition itself is called diverticulosis.
This condition affects about half the people over the age of 60, although typically they don’t experience any symptoms. However, if they do, usually their symptoms include mild cramps, bloating, or constipation.
Diverticulitis occurs when one or more of those pockets—the diverticula—become inflamed and infected. Typically, this happens when the pockets become blocked with waste, creating a bacteria build-up that causes infection.
There are two forms of diverticulitis. When someone has the acute form of the disease, they may experience one or more severe attacks of inflammation and infection. With the chronic form of diverticulitis, although the infection may clear up, it may never completely subside.
What is Diverticular Disease?
Diverticular disease is a blanket term used to refer to medical conditions affecting the diverticula. So, when we say someone has diverticular disease, they might have any of the following:
- Diverticulosis – This means that small “pouches” have developed in the lining of their bowels.
- Diverticulitis – This is the term that’s used when those pouches become inflamed or infected.
- Diverticular Bleeding – With this condition, someone experiences rectal bleeding. This bleeding occurs when there’s chronic injury to the small blood vessels next to the diverticula.
2. Causes & Symptoms
Is Diverticulitis Hereditary?
Yes, there does appear to be a link between genetics and diverticulitis. After examining the genetic and medical information of over 500,000 people between the ages of 40 and 69, a team of researchers identified genes that seem to play a role in the development of diverticular disease.
Still, genetic link or not, there are steps people can take to reduce their likelihood of developing diverticulitis.
What Are the Symptoms of Diverticulitis?
There are a number of different symptoms of diverticulitis, including:
• Advancing Age – Nausea and Vomiting
• Constipation
• Diarrhea
• Flatulence
• Bloating
• Fever
• Bowel Habit Changes
• Lower Abdominal Pain (usually, although not always, on the left side)
3. Who Gets It / Risk Factors
Who Gets Diverticulitis?
Although very few people develop diverticulosis by the age of 40, about half the people in the US develop pockets in their colon by the time they reach 60. And nearly everyone has them once they’re 80 years old.
Of those people who develop diverticulosis, about 15-20% will go on to experience diverticulitis. About two-thirds of the people with diverticulitis experience mild-to-moderate symptoms. The other one-third experiences more severe, life-threatening symptoms.
Interestingly enough, most people who develop diverticulitis before the age of 50 are men. By contrast, after the age of 50, women are more likely to develop the disease.
What Are the Risk Factors Associated with Diverticulitis?
According to the Mayo Clinic, there are several factors that increase your likelihood of developing diverticulitis, including:
• Advancing Age – Diverticulitis becomes more common as people grow older.
• Obesity – People who are seriously overweight are at greater risk of developing the disease.
• Smoking – Smokers are more likely than nonsmokers to get diverticulitis.
• Inactivity – People who exercise vigorously seem to develop diverticulitis less often.
• Low-Fiber, High-Fat Diet – While the jury’s still out on the role fiber plays in diverticulitis, a low-fiber diet that’s high in animal fat appears to increase the risk of developing the disease.
• Certain Medications – There are some medications that are associated with a greater risk of diverticulitis. These include steroids, opioids, naproxen sodium (Aleve), and nonsteroidal anti-inflammatory drugs, like ibuprofen.
4. Diagnosis & Prevention

How Is Diverticulitis Diagnosed?
Typically, someone with diverticulitis visits a physician because they’re experiencing abdominal pain. To determine the source of the problem, the doctor usually performs a physical exam, followed by one or more of these tests:
• Blood and Urine Tests – These help a doctor determine whether someone’s exhibiting signs of an infection.
• Pregnancy Test – This test rules out pregnancy as the cause of abdominal pain in childbearing women.
• Liver Enzyme Test – Again, this is another test to rule out the various possibilities, like liver-related causes of abdominal pain.
• Stool Test – A stool test rules out infection in people with diarrhea.
• CT Scan – A CT scan is used to determine whether someone has diverticulitis and if so, how severe it is. A scan also helps to guide treatment.
Can Diverticulitis Be Prevented?
Yes, diverticulitis can be prevented, but to do so, you’ll probably need to make some lifestyle changes. For instance, the best way to prevent diverticulitis is to:
• Drink Plenty of Water – At a minimum, you should aim to drink at least eight 8-ounce glasses of water a day.
• Exercise Regularly – Exercise can actually improve the muscles in your intestine! And toned intestinal muscles promote regular bowel movements.
• Don’t Delay – Speaking of bowel movements, don’t delay or ignore the urge to go. When nature calls, answer right away.
• Increase Fiber in Your Diet – To avoid uncomfortable bloat, add fiber slowly by incorporating more whole grains, fresh fruits, and vegetables into your meals. Ultimately, your goal should be to work up to 25-35 grams of fiber a day.
• Prevent Constipation – One way to do this is by consuming prunes, prune juice, or a specially formulated tea. There are also over-the-counter stool softeners, but you’ll want to check with your doctor first before using them long-term.
• Avoid Refined Foods – Refined foods are processed foods that are missing the nutrients they once had. This includes plenty of “white” foods like white bread, white bagels, white pasta, white rice, and white flour. Rather than relying on processed food, aim to shop the perimeter of your grocery store—that’s typically where the healthiest food in the store can be found.
• Add Bulk to Your Intake – Psyllium is a soluble fiber derived from the seeds of a plant mainly found in India, called Plantago ovata. This fiber increases the amount of water in your stool, relieving constipation while making bowel movements softer and easier to pass.
Psyllium is actually the main active ingredient in the laxative, Metamucil, although you don’t need to buy Metamucil to use psyllium. Instead, you can always try adding ground psyllium seed to your diet, for instance by sprinkling it on soup, yogurt, or cereal, or by putting it in a protein shake or fruit smoothie.
5. Treatment & Management

Are There Any Natural Remedies to Prevent or Treat Diverticulitis?
Yes, probiotics are useful in the prevention and treatment of diverticulitis.
To explain why that is, it’s helpful to understand how the gastrointestinal (GI) tract works. The GI tract is a muscular tube ~30 feet in length, running from the mouth to the anus. It’s responsible for breaking down food and beverages into smaller molecules, so the blood can absorb them.
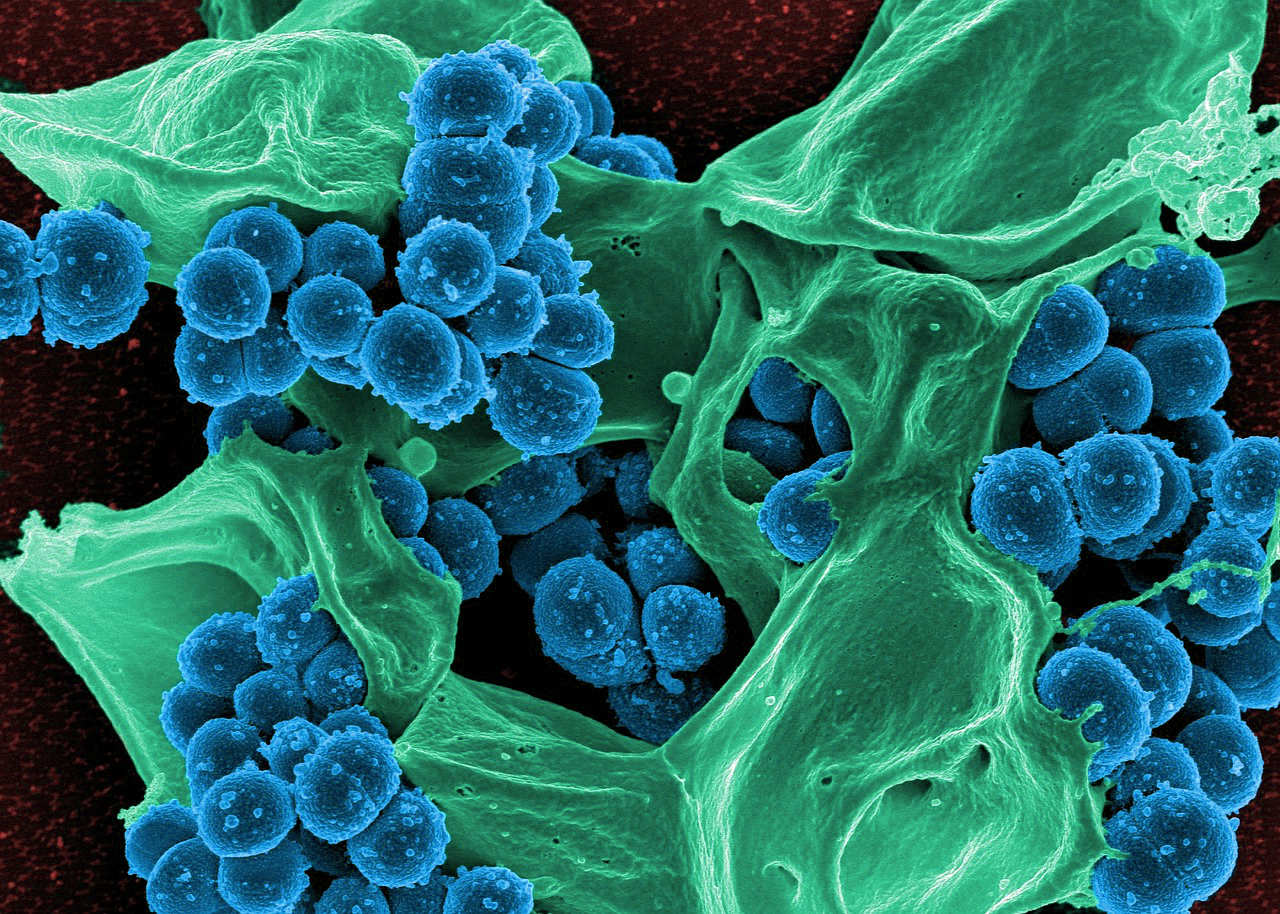
Within the GI tract, there are trillions of bacteria, fungi, viruses, and even parasites—collectively, these are known as microbes. When microbes become out of balance, for example, when there’s an overabundance of “bad” bacteria, the condition’s called dysbiosis.
While researchers still don’t know definitively what causes diverticulitis, they’ve discovered that people with the disease often have dysbiosis.
Additionally, there have been a number of important studies showing that, by improving the bacterial balance in the gut, patients with diverticulitis can prevent flare-ups of the disease and decrease symptoms of abdominal pain and bloating.
So, to up your probiotic intake, choose fermented foods like sauerkraut, kimchi, and kombucha, while opting for a probiotic supplement. Ideally, you’ll want one that contains Lactobacillus casei or paracasei (5 to 25 billion CFUs/day). CFUs, or Colony Forming Units, are a way of measuring the number of live bacteria in a supplement.
Vitamin D also can help with diverticulitis, as it’s been shown to control inflammation in the colon and keep the gut’s lining healthy. However, only a blood test can show whether you’re deficient in Vitamin D.
If you are, it’s a good idea to take a vitamin D3 supplement at a dose of around 5,000 IUs per day to reach a level of 50ng/mL in the bloodstream.
Vitamin D also can help with diverticulitis, as it’s been shown to control inflammation in the colon and keep the gut’s lining healthy. However, only a blood test can show whether you’re deficient in Vitamin D.
If you are, it’s a good idea to take a vitamin D3 supplement at a dose of around 5,000 IUs per day to reach a level of 50ng/mL in the bloodstream.
Can Diverticulitis Be Cured?
Diverticulosis, which is the formation of protruding pouches in the intestines, is incurable. Once one of these protrusions has formed, it’ll remain permanently, and the intestinal wall won’t revert back to its original shape.
We say that someone has diverticulitis when one or more of those pouches become inflamed or infected. While this condition can often be treated with bed rest, stool softeners, medications, and a restrictive diet, patients do run the risk of experiencing another flare-up at some point in the future.
However, they can minimize the likelihood of a reoccurrence by drinking plenty of water, choosing fiber-rich foods, exercising regularly, getting enough Vitamin D, and taking a high-quality probiotics supplement.
What Foods Can I Eat with Diverticulitis?
While you should always consult with your doctor on this subject, a flare-up of diverticulitis typically requires a very restricted diet—at first. Then, over time, you’ll slowly begin to add more foods back into your diet.
Generally, this occurs in the following stages:
Stage 1 – Clear Liquid Diet
During this stage, you’ll allow your digestive system to rest, while you reduce fecal waste with a clear liquid diet, consisting of things like:
• Chicken, Bone, or Vegetable Broth
• Tea
• Strained Lemonade
• Plain Gelatin
• Light-Colored Juices (i.e. Apple)
6. Conclusion
In the United States, thousands of people are diagnosed with diverticulitis each year, and one study suggests the number is on the rise. Unfortunately, even as the number of patients with the disease mounts, there are still plenty of questions doctors and researchers have about the cause of diverticulitis.
However, what they don’t dispute is that diverticulitis flare-ups can be prevented by taking good care of your health. You know the drill—drink your water, up your fiber intake, exercise regularly, and eat fresh fruits and veggies.
You might also consider natural remedies like Vitamin D3, if you have a deficiency, and a probiotic supplement. While probiotics might seem a little “out there,” double blind studies have shown that they’re a safe and effective way to prevent and treat diverticulitis. In fact, a number of so-called “conventional” gastroenterologists recommend them to their patients for that very reason.
By following these simple steps, you can take control of your health, minimizing your likelihood of experiencing future diverticulitis flare-ups. Plus, with the healthy changes you’ve made, you’ll reduce your risk of other serious diseases, so you can “live your best life,” as the kids like to say these days.
FB Comments Will Be Here (placeholder)

CUSTOM JAVASCRIPT / HTML
Related Content
The information presented on this website is not intended as specific medical advice and is not a substitute for professional treatment or diagnosis. These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
*Disclaimer: Results may vary.
© COPYRIGHT Symple Nature LLC. ALL RIGHTS RESERVED.